The thin membrane surrounding the brain and spinal cord is called the arachnoid membrane. Since this membrane resembles a spider web in the microscope, it is called arachnoid membrane, which means spider-like in Ancient Greek.
Arachnoid cysts can develop wherever the arachnoid membrane is present. Arachnoid cysts constitute 1% of intracranial space-occupying formations. In autopsies, this ratio is 1/1000.
They usually show symptoms before the age of 20 and are seen 2-3 times more in boys than girls. In a joint study conducted in Europe, the average age of onset of axes was found to be 6 years.
When and how do arachnoid cysts occur?
The vast majority of arachnoid cysts are congenital. In other words, it occurs with the accumulation of fluid in this region as a result of the separation of the arachnoid membrane in the mother’s womb before birth. At the 15th week of pregnancy in the mother’s womb, cerebrospinal fluid (CSF) begins to circulate under the arachnoid membrane. From this period, there is a possibility of arachnoid cyst development.
It is known to develop less frequently after head trauma (accident, fall) and after brain inflammatory diseases. Arachnoid cysts can develop anywhere in the brain where the arachnoid membrane is present.
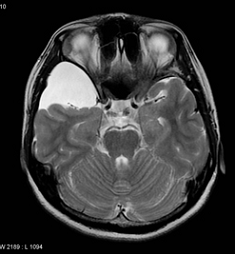
Today, the diagnosis is made by computed tomography (CT) or magnetic resonance imaging (MRI).
What are the Symptoms of Arachnoid Cysts?
Headache and epilepsy are the most common complaints in these cysts. Sometimes they are detected on CT or MRI scans taken for other reasons, although they do not cause any complaints.
Arachnoid Cyst Treatment
Type I cysts should be followed up. Surgery is rarely required. It is necessary to check them with tomography or MR at various times.
Larger Type II and III arachnoid cysts causing Sara (Epilepsy) should be operated on. Bleeding may occur from trauma (fall, beating or traffic accident) into the cyst or between the brain and the thick (dura mater) membrane of the brain.

