Although the etiology of metabolic syndrome is not known exactly, insulin resistance is thought to play a key role. There are various findings showing the relationship of all components of the metabolic syndrome with each other and with insulin resistance.
The frequency of metabolic syndrome increases with advancing age and body weight gain. In the USA, the frequency of metabolic syndrome was found to be 27% in people aged 20 and over, and it was found that the frequency of metabolic syndrome was increasing more rapidly in women. According to the results of METSAR (Turkey Metabolic Syndrome Research) conducted in our country in 2004, the prevalence of metabolic syndrome was found to be 33.9% in adults aged 20 years and over. In this study, the frequency of metabolic syndrome was found to be higher in women than in men. (39.6% for women, 28% for men). In another comprehensive study, TEKHARF (Frequency of Heart Disease and Risk Factors in Adults in Turkey), the prevalence of metabolic syndrome was found to be 28% in men aged 30 and over, and 45% in women. In the TURDEP (Turkey Diabetes Epidemiology) study, diabetes mellitus was found in 7.2% of our adults, glucose intolerance in 6.8%, and obesity in 22% of our adults.
Diagnostic Criteria for Metabolic Syndrome (three of these five conditions make the diagnosis)
1. Waist circumference (abdominal obesity) >88cm in women – >102cm in men
2. Triglycerides > 150mg/dl
3. HDL <40mg/dl in men – <50mg/dl in women
4. Blood pressure >130/85mmHg or hypertension under treatment
5. Fasting glucose >100mg/dl
Obesity is one of the most important components of metabolic syndrome and is closely related to insulin resistance. Obviously, most individuals with the metabolic syndrome are either overweight or extremely obese, and most people with insulin resistance have abdominal obesity.
Insulin resistance, which is frequently seen in type 2 diabetes, can also be seen in individuals with normal glucose tolerance and without diabetes. Detection of insulin resistance in non-obese and non-diabetic relatives of type 2 diabetics supports the role of genetic predisposition. Obesity, sedentary lifestyle, smoking, low birth weight and perinatal malnutrition were also associated with the development of insulin resistance.
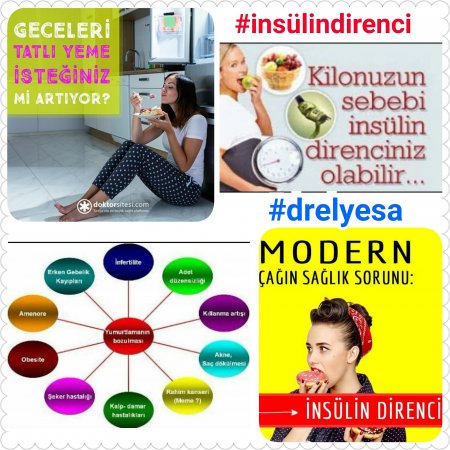
Insulin resistance increasing sympathetic nervous system activation causes hemodynamic disorders such as increased renal sodium retention and increased blood pressure. Approximately 50% of hypertensive patients have insulin resistance. Polycystic ovary syndrome (PCOS) is one of the clinical manifestations with insulin resistance. In addition, nonalcoholic steatohepatitis (NASH) and some cancers may be accompanied by insulin resistance/hyperinsulinemia. Insulin resistance affects the development of atherosclerosis and cardiovascular events independently of other risk factors. It is thought that immunity and inflammation are effective in the pathophysiological role of insulin resistance in metabolic syndrome.
While it is accepted that fasting glucose levels are between 110 and 126 mg/dl in the definition of impaired fasting glucose (IFG), it has recently been suggested that the lower limit be lowered to be between 100 and 126 mg/dl.
Impaired glucose tolerance (IGT), on the other hand, is the 2nd hour values of OGTT between 140 and 200 mg/dl. BAG and BGT can exist together or independently of each other. In these diseases, the risk of developing diabetes mellitus and macrovascular complications is high. About one-third of patients may develop overt diabetes within 10 years. People with normal fasting glucose levels may also have insulin resistance.
Various methods are used in the evaluation of insulin sensitivity. Homeostasis Model Assessment-Homeostasis Model Assesment (HOMA) is currently considered the gold standard. In this method, a single fasting insulin and fasting glucose measurement is sufficient.
HOMA IR=Fasting insulinxfasting glucose/405
A value of 2.5 and above is significant for insulin resistance.
THERAPY:
Large, randomized trials have been published for the treatment of metabolic syndrome. First of all, it should be aimed to correct insulin resistance, which is seen as a basic disorder. In addition, each component of the metabolic syndrome should be controlled separately and diabetes, hypertension and cardiovascular diseases should be prevented or delayed. The primary approach should be the regulation of lifestyle. Weight loss with a suitable nutrition and exercise program provides a corrective effect on all disorders seen in metabolic syndrome. It has been shown that this approach can reduce overall and cardiovascular mortality.
In cases where lifestyle changes are insufficient, the use of agents that increase insulin sensitivity may be considered. Metformin and thiazolidinediones have effects on reducing insulin resistance. It has been shown that the risk of developing type 2 diabetes is reduced with metformin in obese people with glucose intolerance, and with pioglitazone in women with a history of gestational diabetes.
Metformin improves insulin sensitivity at the liver level, while thiazolidinediones are more effective in improving insulin sensitivity in peripheral adipose tissue.
In summary, people who have recently started to gain weight despite not eating much, people who cannot lose weight despite dieting, people whose desire to eat sweets increases excessively and especially at night, people whose hands and feet tremble when they are hungry, people with increased body hair, face and body We recommend that people who have acne in their different parts, women with menstrual irregularity and people with a family history of diabetes should be evaluated in terms of “insulin resistance”.

